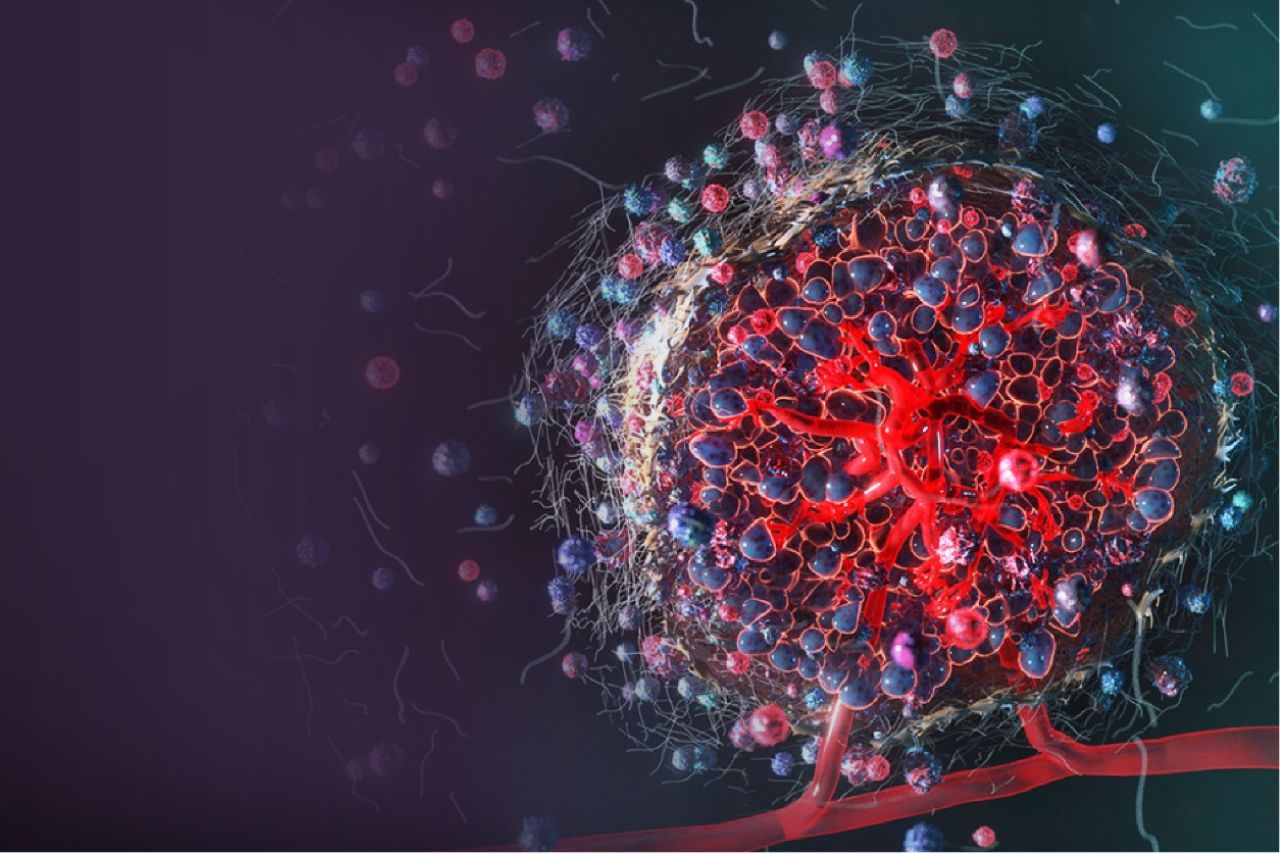
When we talk about non-small cell lung cancer (NSCLC), most people think of tumor cells as the main problem. But in reality, cancer cells are just one part of a larger, highly organized ecosystem: the tumor microenvironment (TME). This microenvironment is made up of structural cells, immune cells, signaling molecules, and even chemical fluctuations like acidity and oxygen levels. Together, these factors determine how tumors grow, spread, and respond to treatment[1].
Recent spatial biology studies have shown that NSCLC tumors contain two broad types of “neighborhoods”. Some areas are rich in immune cells actively fighting the tumor. Others are dominated by stromal and suppressive cells that keep immune cells out, allowing the cancer to thrive. Understanding which are the key players in this environment can reveal why some tumors respond well to therapy while others resist it[2].
Cancer-Associated Fibroblasts: The Tumor’s Structural Architects
One of the most influential cell types in the NSCLC microenvironment is the cancer-associated fibroblast, or CAF. These cells provide structure to the tumor, but they also shape how it behaves. Unlike normal fibroblasts, CAFs secrete signaling molecules such as TGF-B, CXCL12, and VCAM-1, which stiffen the tissue around the tumor, making it harder for immune cells to enter[1].
CAFs don’t come from a single source. They can arise from normal fibroblasts, bone marrow-derived stem cells, epithelial cells, or even from immune cells that change identity under certain signals[1].
CAFS are also a major driver of treatment resistance. They can trigger epithelial-mesenchymal transition (EMT), making cancer cells more invasive and resistant to drugs. Through pathways like YAP/TAZ and the secretion of growth factors such as HGF and IGF1, CAFs reduce the effectiveness of chemotherapy and targeted therapies[1].
Tumor-associated macrophages, or TAMs, are another abundant cell population in NSCLC. These immune cells can either attack tumors or support them, depending on their state. Some TAMs are pro-inflammatory and help T cells infiltrate the tumor. Others adopt a suppressive, “M2-like” role, releasing molecules like IL-10 and TGF-β that weaken immune responses, promote new blood vessel formation, and help tumors spread[2].
Importantly, TAMs and CAFs work closely together. Through chemical signaling loops, they reinforce each other’s suppressive effects. Their collaboration builds physical and immunological barriers that keep killer T cells from reaching tumor cells[2].
Myeloid-Derived Suppressor Cells: Silencing the Immune System
Another key player is the myeloid-derived suppressor cell (MDSC). These cells come in monocytic and granulocytic forms, and their main role in the TME is to shut down the immune attack. They block T-cell proliferation, encourage the expansion of regulatory T cells (which suppress immunity), and release TGF-β and IL-10 to maintain a tolerant, tumor-friendly environment. High levels of MDSCs in the blood are associated with poorer outcomes and lower response rates to immunotherapy.
T Cells: The Immune Frontline
T cells are at the center of the body’s ability to recognize and kill cancer cells. In NSCLC, the spatial distribution of T cells matters. In “immune-rich” zones, cytotoxic CD8 T cells and helper T cells coordinate strong antitumor responses. High numbers of these cells are linked to better survival and better responses to PD-1/PD-L1 checkpoint inhibitors[1].
However, in fibrotic, acidic, or hypoxic areas of the tumor, T cells become exhausted. After prolonged exposure to cancer antigens and suppressive signals, they start expressing molecules like PD-1 and TIM-3, losing their ability to attack. Regulatory T cells (Tregs) further suppress activity by secreting IL-10 and IL-35. Some tumors also contain special immune structures called tertiary lymphoid structures, which are associated with stronger responses to immunotherapy[1].
The Crosstalk
These different cell types don’t act alone. CAFs and TAMs co-regulate fibrosis and suppression through shared hypoxia-driven pathways. MDSCs are recruited by CAFs and contribute to immune silencing. T cells are excluded or exhausted in these fibrotic zones. Hypoxia caused by the dense matrix activates more TGF-β and HIF1a, feeding into the same cycle.
The result is a self-sustaining feedback loop that protects the tumor from both the immune system and therapies. This is one reason why standard treatments can lose effectiveness, particularly in advanced disease.
Targeting Tumor Acidity with L-DOS47
One of the defining features of this hostile microenvironment is its acidity. The extracellular pH in tumor regions can drop below 6.8, compared to the normal physiological pH of around 7.4. Acidic conditions favor tumor invasion, encourage immune suppression, and reduce the potency of therapies. L-DOS47 is an investigational therapy designed to tackle this specific problem. It combines an antibody fragment that targets CEACAM6-a protein commonly found on NSCLC cells with the enzyme urease. Once bound to the tumor, the enzyme converts naturally occurring urea into ammonia and carbon dioxide, locally raising the pH.
By normalizing acidity, L-DOS47 helps restore T-cell function, shifts macrophages toward a more inflammatory state, and disrupts the physical and chemical barriers that tumors use to protect themselves. Early clinical trials in NSCLC have shown that this approach is well tolerated and may enhance the effectiveness of chemotherapy.
A New Way of Thinking About Treatment
The NSCLC tumor microenvironment is not just background tissue. It is an active, evolving network that shapes how tumors grow, spread, and respond to treatment. CAFs create barriers; TAMs and MDSCs suppress immunity; T cells fight back but are often exhausted; acidic and hypoxic conditions raise the barriers to anti-cancer immunity and therapies, making cancers harder-to-treat.
Targeting the metabolic environment, such as through pH modulation with L-DOS47, represents a promising new strategy. By changing the ecosystem rather than just attacking tumor cells, we may be able to turn immunologically “cold,” resistant tumors into more vulnerable ones and improve outcomes for patients with NSCLC.
Ref:
1. Rahal Z, El Darzi R, Moghaddam SJ, Cascone T, Kadara H. Tumour and microenvironment crosstalk in NSCLC progression and response to therapy. Nat Rev Clin Oncol. 2025 Jul;22(7):463-482. doi: 10.1038/s41571-025-01021-1. Epub 2025 May 16. PMID: 40379986; PMCID: PMC12227073.
2. Katarína BalážováHans CleversAntonella FM Dost (2023) The role of macrophages in non-small cell lung cancer and advancements in 3D co-cultures eLife 12:e82998. https://doi.org/10.7554/eLife.82998
One Reply on “The Tumor Microenvironment in NSCLC: A Hidden Force Shaping Cancer Growth and Treatment Response”
Comments are closed.