One of the most consistent hallmarks of cancer biology is the acidity of solid tumors, a characteristic that gives cancer cells a survival advantage. This acidity is not a passive byproduct of cancer metabolism, as was first noted as early as the 1920s with observations of glycolytic metabolism in tumors, but is now understood as an active driver of tumor progression, immune evasion, metastasis, and drug resistance.123
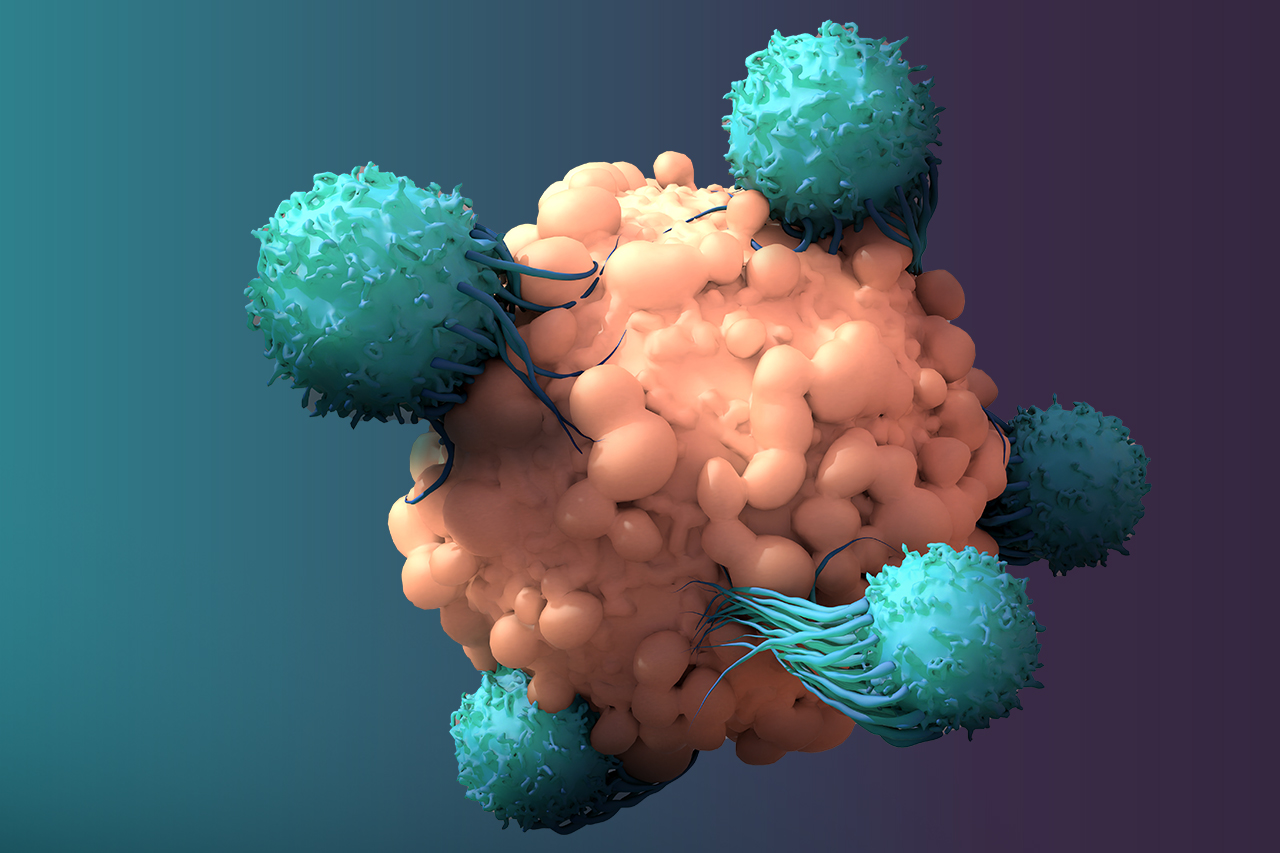
With growing recognition that the tumor microenvironment (TME) is central to therapeutic success, acidity has come into focus as a decisive factor, reshaping not only tumor growth and metastasis but also the tumor immune microenvironment (TIME), where it can dictate the success or failure of cancer immunotherapies.4
In response, a growing body of research has focused on strategies to neutralize tumor acidity and establish a TME more conducive to therapy. Approaches such as systemic buffering agents and inhibitors of acid transport have been explored, but their clinical translation has been limited by challenges in achieving effective and sustained alkalization.123
Efforts to overcome these barriers have given rise to a new generation of tumor-targeted therapies that seek to directly remodel the acidic TME. Among them is Helix BioPharma’s Tumor Defense Breaker™ L-DOS47, a first-in-class antibody-enzyme conjugate (AEC) designed to locally convert urea into ammonia, raising pH within the TME and re-sensitizing tumors to cancer immunotherapies.
Why Acidity Matters in Cancer
Most healthy tissues in the body maintain a tightly regulated extracellular pH (pHe) of 7.2 to 7.4. By contrast, solid tumors often display pHe values ranging from 6.5 to 6.9.12
This acidification arises from a phenomenon known as the Warburg Effect, in which tumors preferentially generate energy by breaking glucose into acidic lactate through glycolysis, even in the presence of oxygen and functional mitochondria.125
When coupled with dysfunctional vasculature, the result is a buildup of hydrogen ions that drives a persistently acidic environment in and around tumor cells.135
The acidic TME drives cancer progression by selecting for more aggressive, therapy-resistant clones.123
At the same time, low pH activates enzymes that degrade the extracellular matrix, breaking down the physical barriers around the tumor and allowing cancer cells to invade surrounding tissue and metastasize.125
Acidity also switches on angiogenic signals such as VEGF, which drive the formation of abnormal new blood vessels, fueling hypoxia, acid production, and tumor expansion.125
It blunts immune surveillance, co-opting immune cells to suppress the activity of cytotoxic T cells (the immune system’s frontline fighters), disrupts T cell motility and competes for glucose with tumor-infiltrating T cells, leading to their exhaustion and driving tumor progression.46
The result is a competitive advantage for the tumor and a hostile setting for therapy.1236
Beyond Buffering: Pharmacologic Approaches to Tumor Alkalization
Neutralizing tumor acidity through the oral administration of buffers like sodium bicarbonate has shown promise in preclinical models.127
Studies have demonstrated that buffering can reduce metastasis and enhance the efficacy of checkpoint inhibitors in animal models of melanoma and pancreatic cancer.127
This has driven interest in alternative alkalization strategies:
- Proton transport inhibitors (PTIs): Agents targeting proton pumps (e.g., V-ATPase inhibitors) or transporters (e.g., Na⁺/H⁺ exchangers, monocarboxylate transporters [MCTs]) reduce extracellular acidification by blocking H⁺ efflux. While effective in preclinical studies, most PTIs have faced hurdles in systemic toxicity and poor selectivity for tumor cells, limiting clinical adoption.123
- Nano-enabled extracellular alkalization: Nanoparticles engineered to release buffering agents (e.g., calcium carbonate, magnesium hydroxide) within the TME can locally raise pHe. These nanoplatforms also allow co-delivery of chemotherapeutics, enhancing drug uptake in an alkalized tumor milieu. However, scalability, biocompatibility, and controlled biodistribution remain challenges.7
- Enzymatic and metabolic interventions: Inhibition of lactate dehydrogenase (LDHA) reduces lactate accumulation and indirectly alleviates extracellular acidification. While promising, systemic LDHA inhibition risks toxicity to normal tissues that also rely on glycolysis.356
- Intracellular acidification approaches: Complementary to TME alkalization, some investigational strategies aim to selectively lower the intracellular pH (pHi) of cancer cells. This exploits the fact that tumor cells maintain an alkaline cytosol (pHi ~7.4–7.6) as an adaptive survival mechanism. Pharmacologic inhibition of proton exporters or delivery of acid-generating nanoparticles can collapse this gradient, triggering apoptosis or necrosis. This “inside-out” strategy remains experimental but highlights the broader therapeutic potential of targeting tumor pH dysregulation.37
Collectively, these findings underscore both the promise and the limitations of current alkalization therapies. Most approaches have been challenged by lack of tumor selectivity, systemic side effects, or delivery issues fueling the need for more precise solutions.1237
Why Pharmacological Alkalization Works
Neutralizing tumor acidity offers several benefits, all of which align with known hallmarks of cancer:
- Immune restoration: Acidic conditions suppress T-cell function by impairing cytokine secretion and downregulating key surface receptors. Buffering the TME restores the ability of T cells to recognize and attack tumor cells, thereby improving immunotherapy efficacy.46
- Reduced invasion and metastasis: An acidic pH promotes protease release and matrix remodeling, enabling tumor cells to invade nearby tissues. Alkalization inhibits this process and can reduce the likelihood of distant spread.1235
- Overcoming drug resistance: Many chemotherapeutics are weak bases that become protonated and trapped in the extracellular space or lysosomes. A neutralized TME enhances drug penetration and intracellular retention.1237
- Targeting metabolic vulnerabilities: Tumor cells adapted to acidic pH show specific metabolic dependencies (e.g., glutamine metabolism, lipid synthesis). By altering the pH, these vulnerabilities may be exposed and therapeutically exploited.36
A Smarter Strategy: Tumor-Targeted Alkalization
L-DOS47 is a fusion of a camelid-derived single-domain antibody (nanobody) targeting CEACAM6 (an antigen overexpressed in many solid tumors), and the enzyme urease, which converts endogenous urea into ammonia and bicarbonate.4
Once administered intravenously, L-DOS47 navigates through the bloodstream to locate and bind with CEACAM6-expressing cancer cells.4
Upon binding, the urease component becomes catalytically active within the acidic TME, locally converting urea into two molecules of ammonium and one molecule of bicarbonate.4
Recent evidence suggests that the cytotoxic effect of ammonia is highly dependent on the extracellular pH. At higher pH levels, a greater fraction of ammonia exists in a membrane-permeable form, enhancing its ability to enter cells, disrupt organelle function, and suppress tumor growth.3
In parallel, the generation of bicarbonate at the tumor site contributes to raising extracellular pHe, which not only counteracts tumor acidity but also improves therapeutic responsiveness.4
A more alkaline microenvironment increases the activity of ionizable, weak-base chemotherapeutics such as doxorubicin by facilitating their penetration into cancer cells, while also promoting infiltration and activation of immune populations including T cells, B cells, and macrophages.7
The result is a highly localized increase in pHe in the tumor microenvironment.4
By bypassing systemic buffer delivery, L-DOS47 offers an elegant and targeted way to neutralize tumor acidity at the source.4
How L-DOS47 Stands Apart
Unlike systemic buffers, PTIs, or nanoparticle approaches, L-DOS47 uniquely combines tumor antigen targeting with enzyme-driven alkalization. Its localized activity avoids systemic pH disruption, patient compliance barriers, and high-dose regimens required for oral buffers.4
CEACAM6 provides an ideal target because it is not only highly expressed in multiple aggressive tumors (e.g., NSCLC, PDAC, CRC where therapeutic options remain limited), but also implicated in immune evasion and resistance pathways. Importantly, CEACAM6 blockade itself may confer therapeutic benefit: disruption of CEACAM6–CEACAM1 interactions has been shown to enhance T cell responses, suggesting that L-DOS47 nanobody binding could offer dual benefits—enzyme delivery plus partial immune reactivation.4
Safety and tolerability have been demonstrated in early Phase I/II NSCLC trials, with encouraging signals of efficacy in chemotherapy combinations.4
L-DOS47 has already demonstrated safety and tolerability in Phase I/II trials in NSCLC, with promising signals of efficacy when combined with chemotherapy.4
A Platform for the Future
L-DOS47 is more than a single asset; it is proof of concept for pharmacological alkalization. It opens the door for a new class of therapies that don’t just attack the tumor directly but reshape its surroundings to enable better outcomes from existing treatments.
As immunotherapy and precision oncology continue to evolve, so must our approach to the tumor microenvironment. Targeting cancer’s hidden enablers like acidity represents a bold, science-driven path forward. By unlocking tumors from within, therapies like L-DOS47 hold the promise to turn resistance into response and the intractable into treatable, toward more durable, accessible, and effective cancer care.
References:
1 Hamaguchi R, Isowa M, Narui R, Morikawa H, Wada H. Clinical review of alkalization therapy in cancer treatment. Front Oncol. 2022;12:1003588.
2 Ibrahim-Hashim A, Estrella V. Acidosis and cancer: from mechanism to neutralization. Cancer Metastasis Rev. 2019;38(1-2):149–55.
3 Pillai SR, Damaghi M, Marunaka Y, Spugnini EP, Fais S, Gillies RJ. Causes, consequences, and therapy of tumors acidosis. Cancer Metastasis Rev. 2019;38(1-2):205–22.
4 Tang T, Huang X, Zhang G, et al. Advantages of targeting the tumor immune microenvironment over blocking immune checkpoint in cancer immunotherapy. Signal Transduct Target Ther. 2021;6(1):72.
5 Kato Y, Ozawa S, Miyamoto C, et al. Acidic extracellular microenvironment and cancer. Cancer Cell Int. 2013;13:89.
6 Najdi R, et al. Microenvironmental metabolism regulates anti-tumor immunity. Cancer Res. 2019;79(4):793–801.
7 Yang Y, et al. Sodium bicarbonate nanoparticles modulate the tumor pH and enhance the cellular uptake of doxorubicin. J Control Release. 2019;296:73–82.